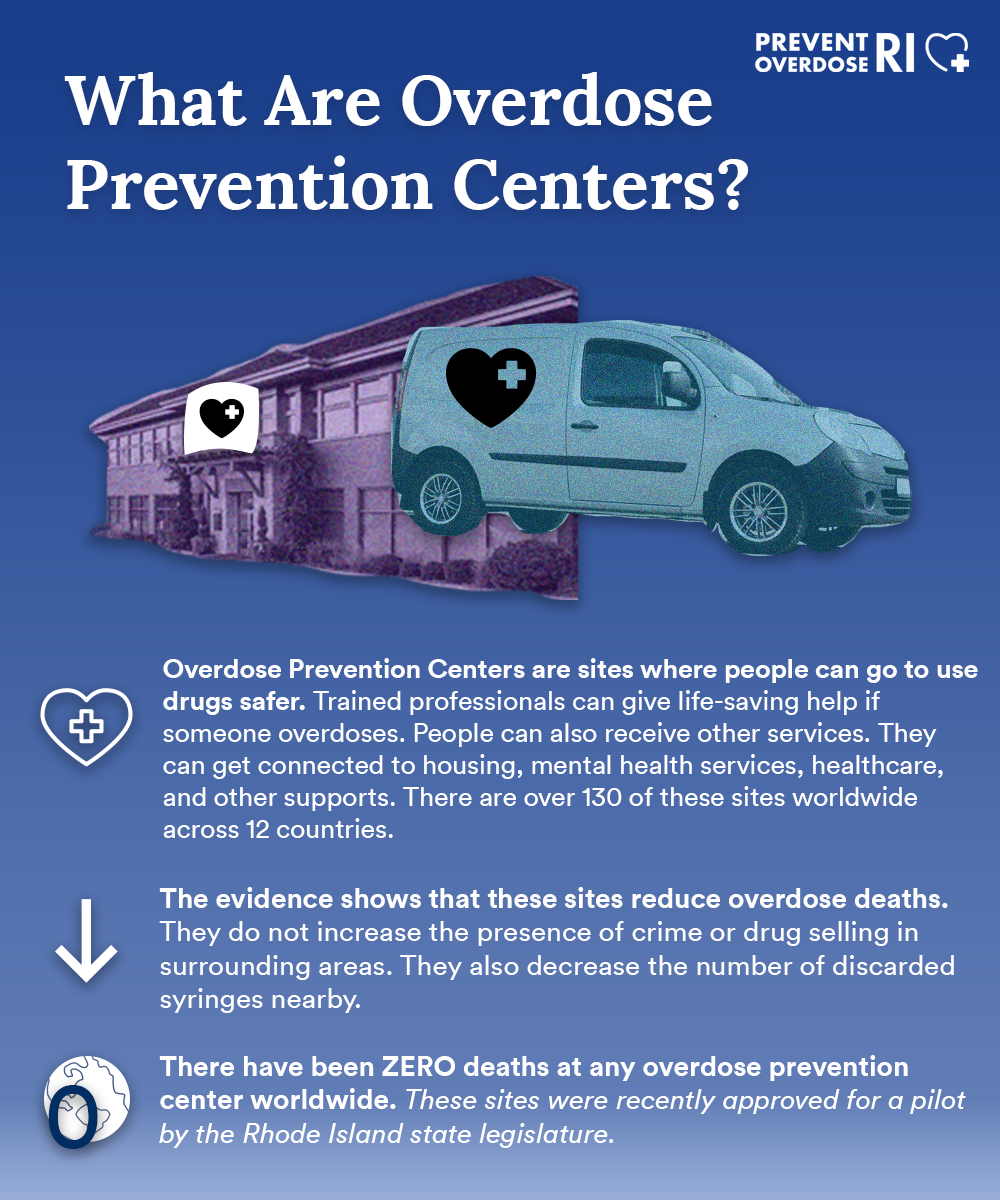
Overdose prevention centers (OPCs) (sometimes called safe consumption sites, safe injection sites or drug consumption rooms) are safe, monitored spaces where trained staff can intervene in the event of an overdose.
In 2021, 435 Rhode Islanders lost their lives due to an accidental drug overdose. Many overdoses happen when people are alone. When people are alone, no one can call 911 or administer naloxone, a drug that can reverse an overdose. We need more ways to stop these deadly overdoses. In OPCs, trained staff can use naloxone (an overdose reversal medication) and oxygen to reverse an overdose and save a life, without needing to call 911.
There is currently one overdose prevention center operating in the state, operated by Project Weber/RENEW in Providence. These sites are regulated by the Rhode Island Department of Health and have been approved by the Rhode Island State Legislature.
Get Involved
How do Overdose Prevention Centers work?
They reduce overdose deaths.
These sites reduce overdose deaths in the neighborhoods they are located in. One study from Vancouver showed a 35% drop in overdose deaths in the area where the OPC opened. In Toronto, there was a 69% drop in overdoses within 1000m of overdose prevention centers one year after they opened. They prevent overdoses by having staff readily available to address emergencies, and foster an environment that increases the safety and security of participants, even when they are not using an OPC. For example through naloxone distribution and having trained staff available.

They connect people to treatment.
These sites also connect people to treatment. Research shows that using an OPC increases the amount of people who use treatment services like medication assisted treatment. At OPCs there are often counselors on site, some of whom are peers. Research shows these counselors are effective at helping people get into treatment. One study found that 42% of opc participants not previously enrolled in treatment were enrolled within two years of using the OPC.
They save communities money.
OPCs save cities money. They reduce the amount of overdoses and infections. Studies have looked into the cost-effectiveness of these sites across different American cities. These studies have all found reduced healthcare costs. There are fewer visits to the emergency room, fewer ambulance rides, and fewer hospital stays. This saves money and reduces the burden on emergency service staff. By giving out safe supplies and teaching people about using safely, the risk of infections like HIV can be reduced. Furthermore, these infections can need years of treatment, which can be costly.
They reduce litter and don’t increase drug use.
By offering a safer place to use drugs, these sites also keep the community safe. OPCs provide a place to dispose of needles and other used drug equipment, which decreases the amount of litter on the street. One study found a drop in public drug use 12 weeks after an OPC opened in Vancouver. Studies have also shown that these sites do not increase drug use or drug selling activity in the area. There are also no increases in violent crimes like assault or robbery. In fact, one study looked at an unsanctioned site in the US for five years and found that there was a decrease in crime.
They reduce infections.
OPCs reduce the spread of HIV and other infectious diseases. They provide access to basic healthcare, sterile supplies, and spread knowledge on safer drug use practices. Research has estimated that these sites reduce HIV infection rates by 6%-11% amongst those who use them. Studies have also shown that using these sites reduces the risk of getting abscesses. People are also more likely to seek treatment for drug-related skin injuries (like soft tissue infections) at these sites compared to a hospital. People who use these sites are also likely to report using harm reducing approaches including using new syringes when they use drugs. Data from one site in the US shows that those who used an OPC were less likely to go to the emergency room and the hospital.
What does an overdose prevention center look like?
Take a tour of the Overdose Prevention Center in New York City.
Watch this video from opcinfo.org which tours the Overdose Prevention Center in East Harlem, New York City, operated by OnPoint NYC.
Ashley Perry, Co-Director of the Overdose Prevention Center in Providence talks about these sites.
Watch this video from Filter Magazine, where Ashley Perry, Co-Director of the Overdose Prevention Center in Providence talks about how OPCs work, why they are needed and the work they do every day.
How will we know if the site in Rhode Island is effective?
There is currently an ongoing study that is evaluating the effectiveness of this site and the sites in New York City. The study is conducted by a team at New York University and Brown University. You can find out more about the study and learn more about their results here.
Download Fact Sheets
There is a lot of scientific evidence on overdose prevention centers. opcinfo.org has created fact sheets that summarize this research based on different topics.

Community Impacts
Find out more about the impacts that overdose prevention centers have on the surrounding community.
Operational Considerations
Read more about the operational considerations that go into operating an overdose prevention center.
Social media graphics
Download and share graphics that explain the concept of overdose prevention centers.
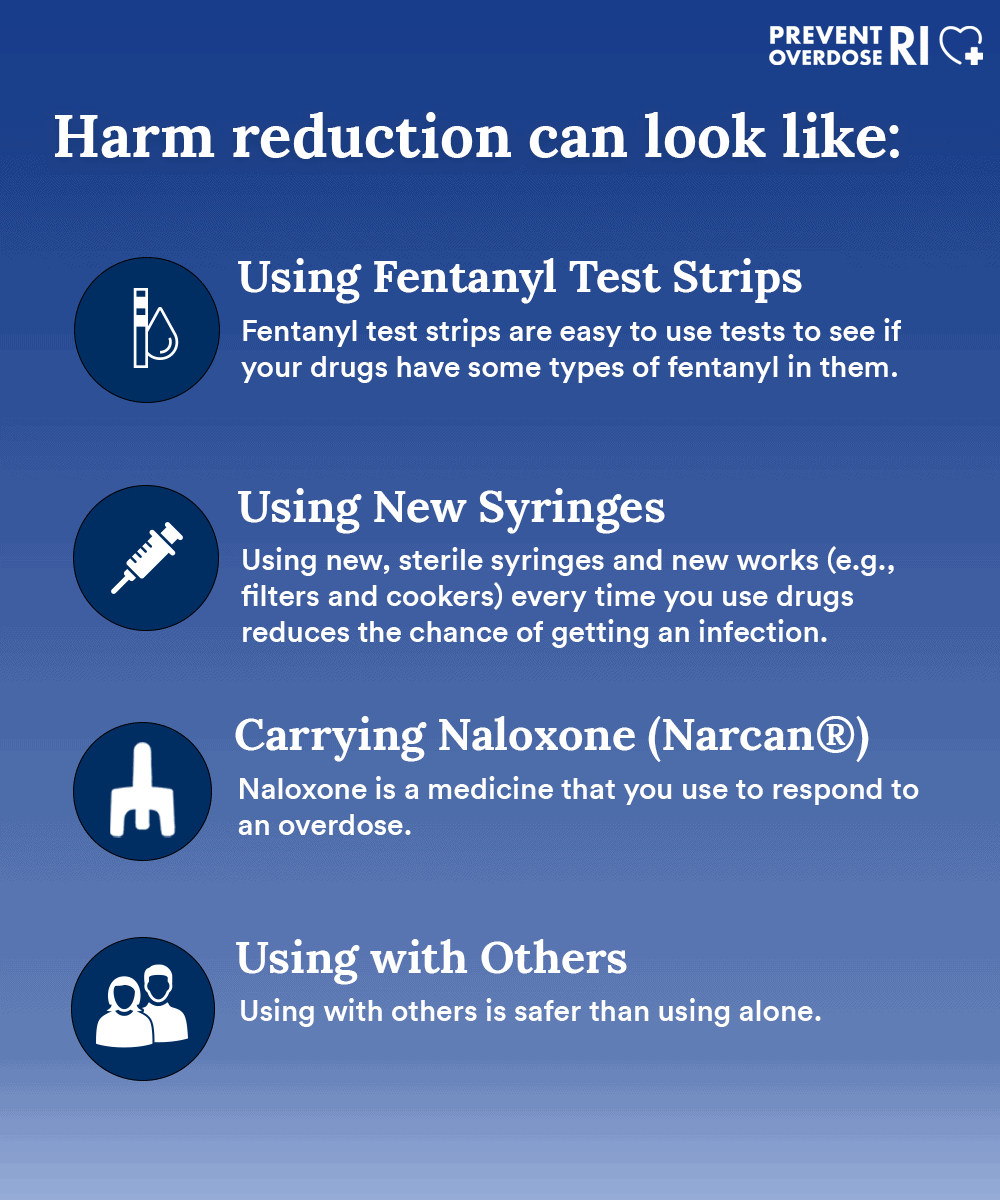
Harm reduction can keep us safe

What does harm reduction look like?
What are overdose prevention centers?
Harm reduction keeps people alive.
More Resources
Resources for safer drug use
In Rhode Island, you can already get supplies and services to stay safer when you use drugs. Find out where you can get syringes, naloxone, fentanyl test trips, and get tested for HIV and hepatitis C.
Safer drug use practices
Learning to take care of yourself takes time and thought. There are many that you can do to help you use drugs more safely. This includes resources in the community that you can access, as well as general suggestions to prevent overdose and infection.